Today might just have been the coolest day that I’ve ever experienced up to date. Jonathan and I didn’t actually start the day at Carolina Ear and Hearing Clinic though; instead we woke up at 6:00 to shadow Dr. McElveen in an operating room at Duke Raleigh Hospital. When we arrived, we scrubbed up and received our official name tags to then follow Dr. McElveen to an operating room where he would preform a tympanoplasty operation.

In the operating room, Dr. McElveen explained to us that the patient’s ear drum had collapsed when her Eustachian tube (a passage that permits the equalization of pressure on both sides of the ear drum) acted as a vacuum and sucked the ear drum in on itself. The collapse caused a tear in the ear drum, so the patient had a large hole in it. To correct this, Dr. McElveen cut cartilage away from the back of the patient’s ear and augmented it to her ear drum to patch up the hole.
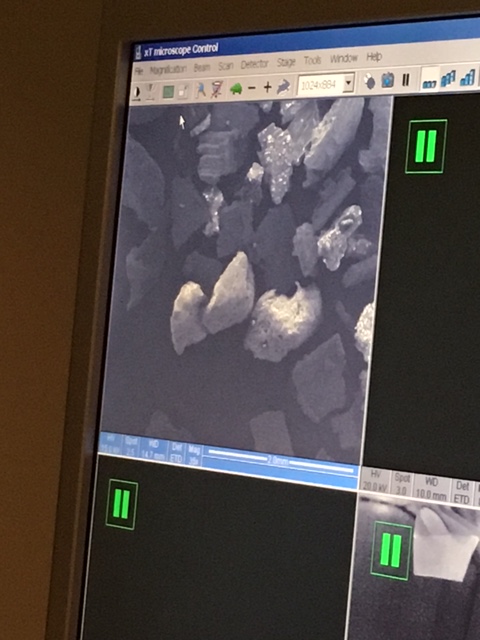
The “middle ear” of the patient during surgery, showing the stapes and incus bones as well as the folded-back tympanic membrane:

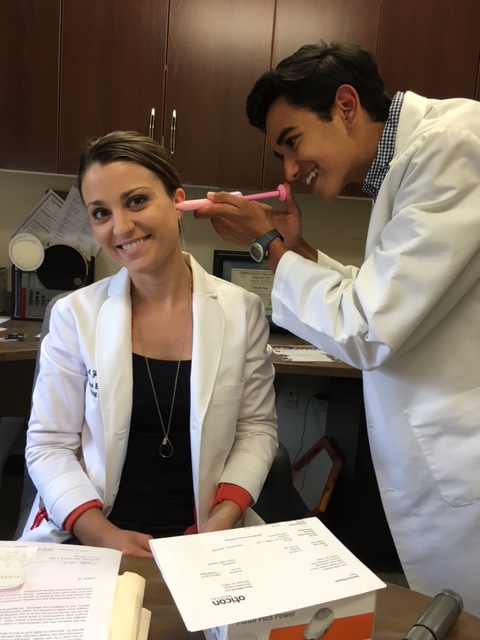
After the successful surgery ended, we celebrated with some pictures with Dr. McElveen and in our scrubs:

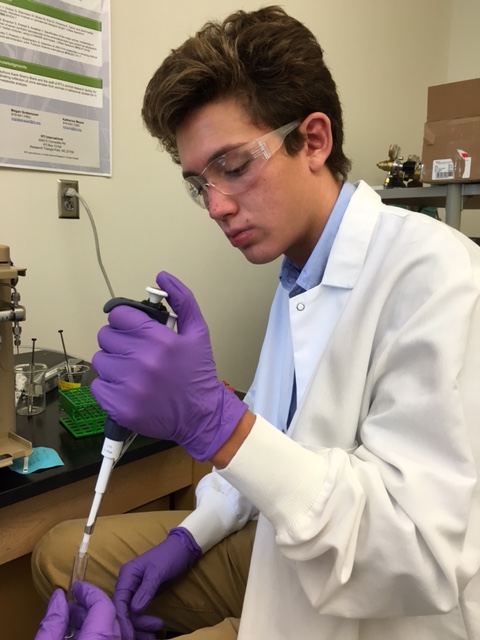
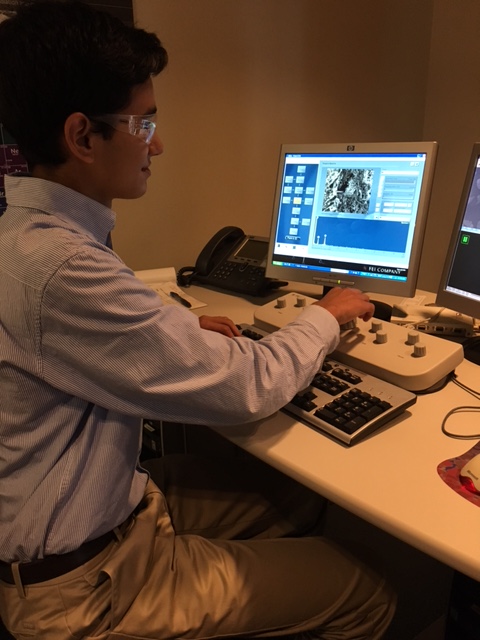
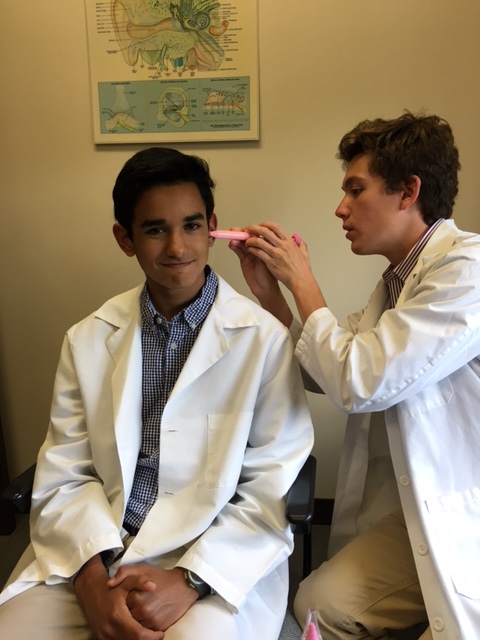
We then headed back to the Carolina Ear and Hearing Clinic where Dr. McElveen set Jonathan and me up in the clinic’s temporal bone lab. He let us probe a temporal bone and it’s ear cartilage, and it was really cool! However, we did find out how hard it is to actually be a surgeon from this because of how precise your instruments need to be held, and how hard it is to keep your hands from shaking when probing the patient’s body. The ear canal is so narrow that I felt like I was playing Operation since I wasn’t supposed to shake the probe and touch the sides of the canal!
Dr. McElveen demonstrating how to probe the temporal bone in the bone lab:

Jonathan probing the temporal bone:

After we (half) successfully probed the temporal bone and the ear cartilage, we had our lunch break. After lunch, Dr. McElveen had to leave to go to South Carolina to perform a surgery there. Thus, Jonathan and I separated and I went with one of the audiologists to examine a patient with a tumor on their hearing nerve called an acoustic nueroma. She conducted several tests on the patient in order to determine whether it was worth it for Dr. McElveen to attempt to save the patient’s hearing capability in the ear and remove the tumor, or if he should just incise the hearing nerve in order to remove the tumor, which would ultimately render the patient deaf in the one ear. One of the tests was to lay the patient down in a dark room and put plugs in her ears that would send sounds through her nerves and a machine would measure how long it took the brain to receive the sound. The patient had to lay completely still so that all of the body’s focus would be on delivering those sounds to her brain. Apparently she was laying so still that she actually fell asleep during the test! This was okay though according to the audiologist because the data still comes back accurately. After several tests, the audiologist determined that it would not be worth it for Dr. McElveen to attempt to save the patient’s hearing capability.
Today was such an amazing experience since we did so much observing and hands-on activities! I will never forget being in that operating room and observing the surgery; my jaw was dropped the whole time as I was in such awe of what Dr. McElveen was doing throughout the operation! It was also a very formative experience, and it definitely sparked my interest in possibly going into surgery as a career option. – Kiran W.