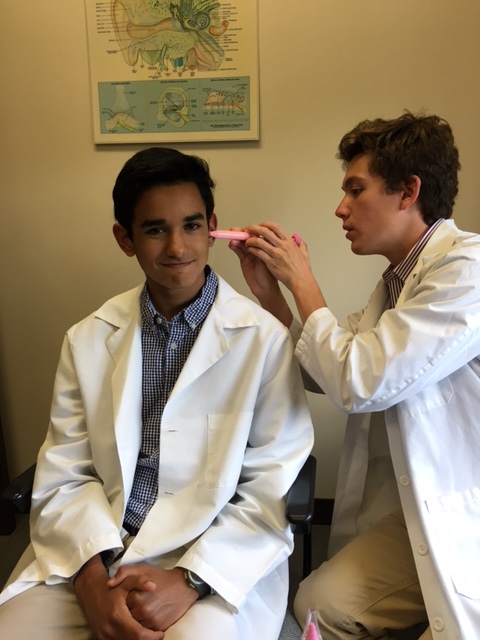
This morning was awesome because 1. Jonathan and I didn’t have to be at the office until 9:00 and 2. we got to learn how to operate the hearing test machines and conduct hearing tests on each other! First we examined each other’s ears with an otoscope to make sure that nothing was in the ear canal that would block sound from entering and reaching the ear drum, such as ear wax.
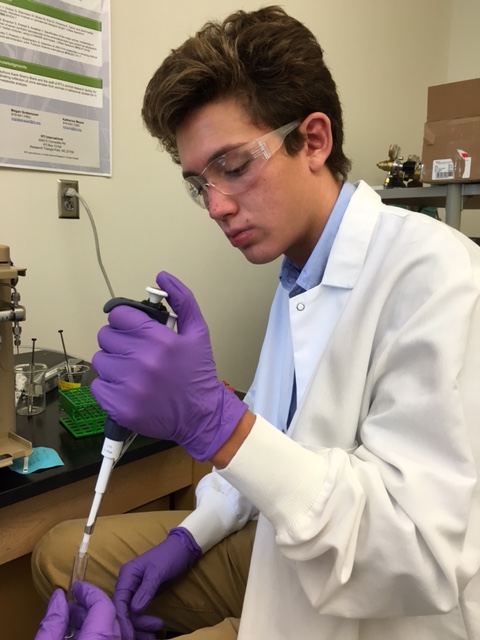
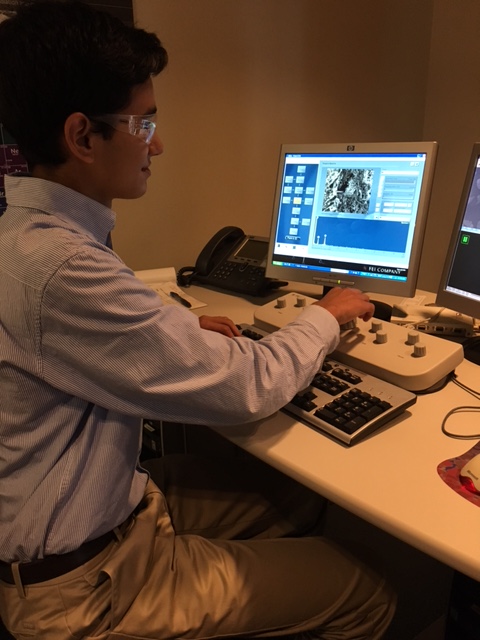
Me examining Jonathan’s ear canal with an otoscope:

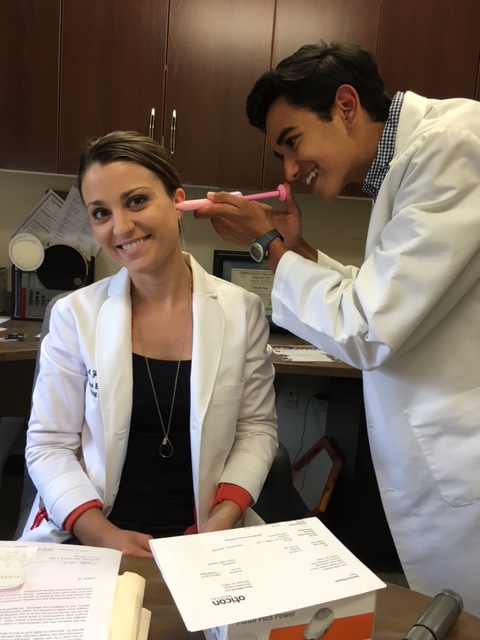
Jonathan goofing around while I looked into his ear canal:

After we got the “all clear” from each other that our ear canals were clean, one of us headed to another room where the hearing test machine was located so that the “patient’s” room was completely silent and no sound would interfere with their hearing test. To conduct the hearing test, you start the sound at a certain frequency in only one ear, and change the amount of decibels each time. If the patient responds to a sound by pressing a button, you decrease the amount of decibels by 10. If the patient does not hear the sound, you increase the amount of decibels by 5 until the patient is consistently hearing a certain number of decibels at the one frequency. You chart this number and then change the frequency and start again until the chart is completed. After the chart is complete, you have the hearing test complete for the one ear, so you switch to the other ear and repeat.
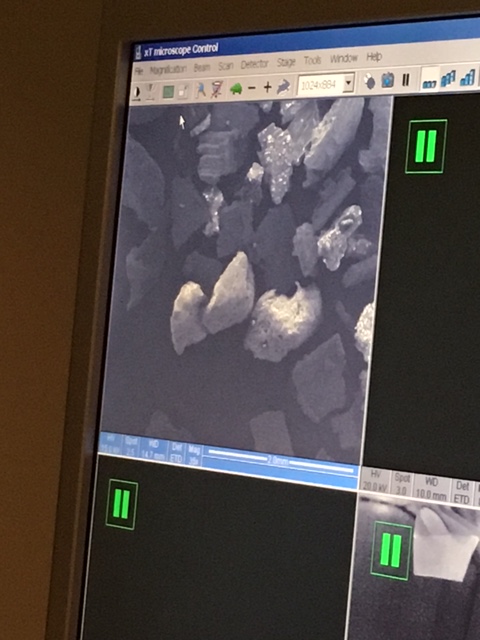
Pausing during my hearing test for a quick selfie. In the picture the top left number is the decibel amount for the one ear (15 dB) and the middle number is the frequency (1000 Hz).:

After our hearing tests, our charts determined that Jonathan had normal hearing; however, he couldn’t hear the lower frequency sounds when the decibel amount was too low, while I had perfect hearing and was able to hear all of the frequencies even at 0 decibels (subtle brag… Jonathan was a little jealous of this).
Our completed hearing charts. Jonathan’s hearing chart is the one on the left while mine is on the right. Patients who come in with hearing loss will typically have points that are more towards the middle of the chart.:

After our hearing tests, we had our lunch break followed by some routine hearing aid checkups. Many of the patients that the audiologist and I saw were participating in a study with a new type of hearing aid that sends a laser light down the ear canal that hits a light receptor on what was described as “a contact lens for the ear drum” which causes a motor to vibrate the ear drum and allows that patient to hear. This new technology is very advanced and groundbreaking.
Overall today was a very fun and informative day as we learned about a lot about the technology that audiologists use in the current day and age. I especially enjoyed being able to conduct the hearing test on Jonathan, and the audiologists told us that tomorrow we would be able to do more experiments on each other using different types of technology. I can’t wait! – Kiran W.